Impact
THE BOGALUSA HEART STUDY
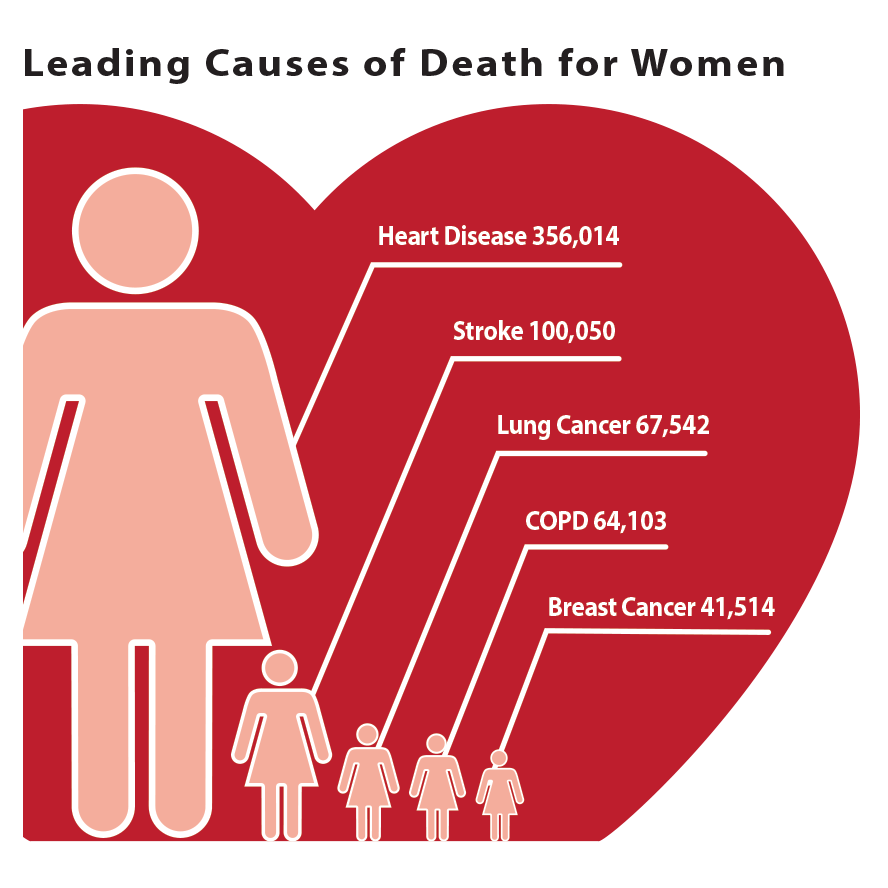
2022 Leading Causes of Death
Heart Disease
Cancer
Injury
Covid 19
Pediatric Guideliness for Blood Pressure
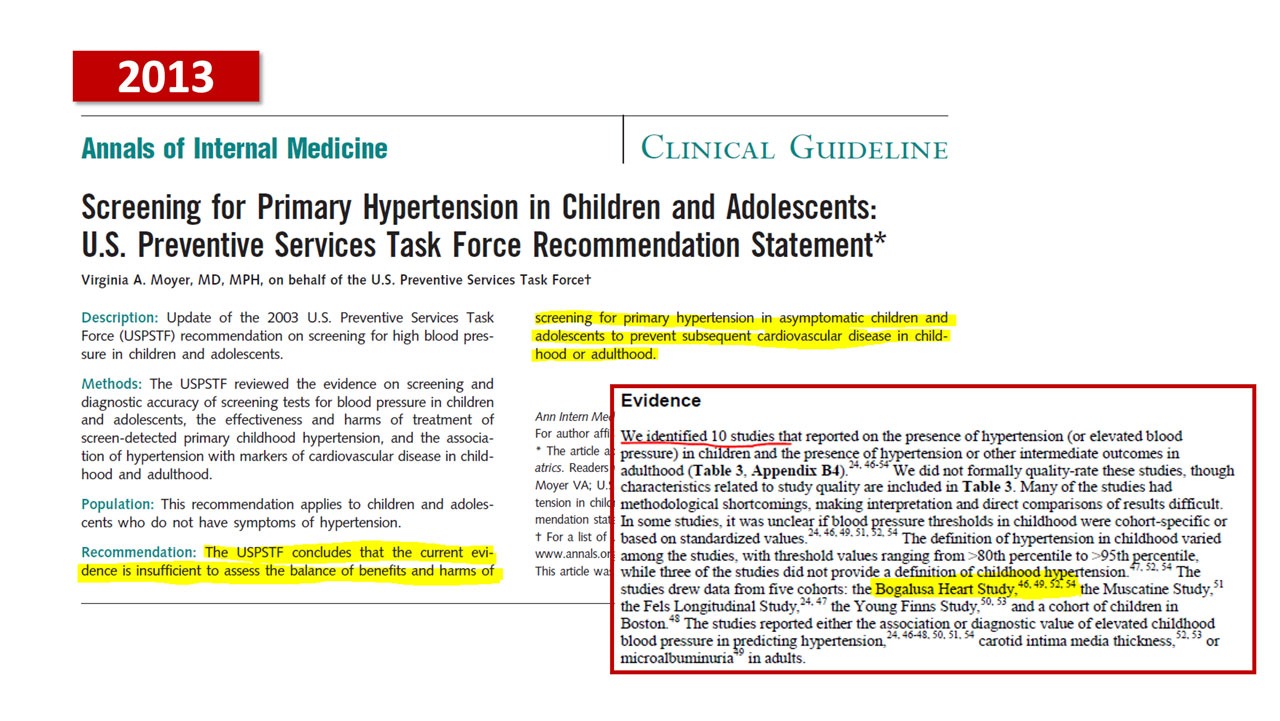
Pediatric Clinical guidelines for blood pressure still do not recommend measuring blood pressure in children because there is insufficient evidence that it can prevent the development of heart disease and premature death in adulthood. This is because the gold standard type of evidence on this topic, a randomized controlled clinical trial that spans 40 or more years is too expensive and impractical to ever conduct. The next best type of evidence is the kind supplied by the Bogalusa Heart Study, long-term follo-up of children with measurements of blood pressure made throughout the lifespan into adulthood.
The Bogalusa Heart Study, at 50 years, has the most evidence of any US study measuring blood pressure throughout lifespan, which makes the contribution of the people of Bogalusa so unique and profound.
The evidence from the Bogalusa Heart Study and other studies that are part of the International Childhood Cardiovascular Cohort Consortium (i3C add link) is the only information of its kind that can answer this question, and change clinical guidelines to improve the health of our children for generations to come.
Pediatric Clinical guidelines for blood pressure still do not recommend measuring blood pressure in children because there is insufficient evidence that it can prevent the development of heart disease and premature death in adulthood.
Weight of the Nation

Weight of the nation, features NIH research conducted in part in of Bogalusa
In this four-part documentary series HBO highlights how obesity is one of the biggest threats to American health and features the Bogalusa Heart Study prominently.
Recent Results and Discoveries
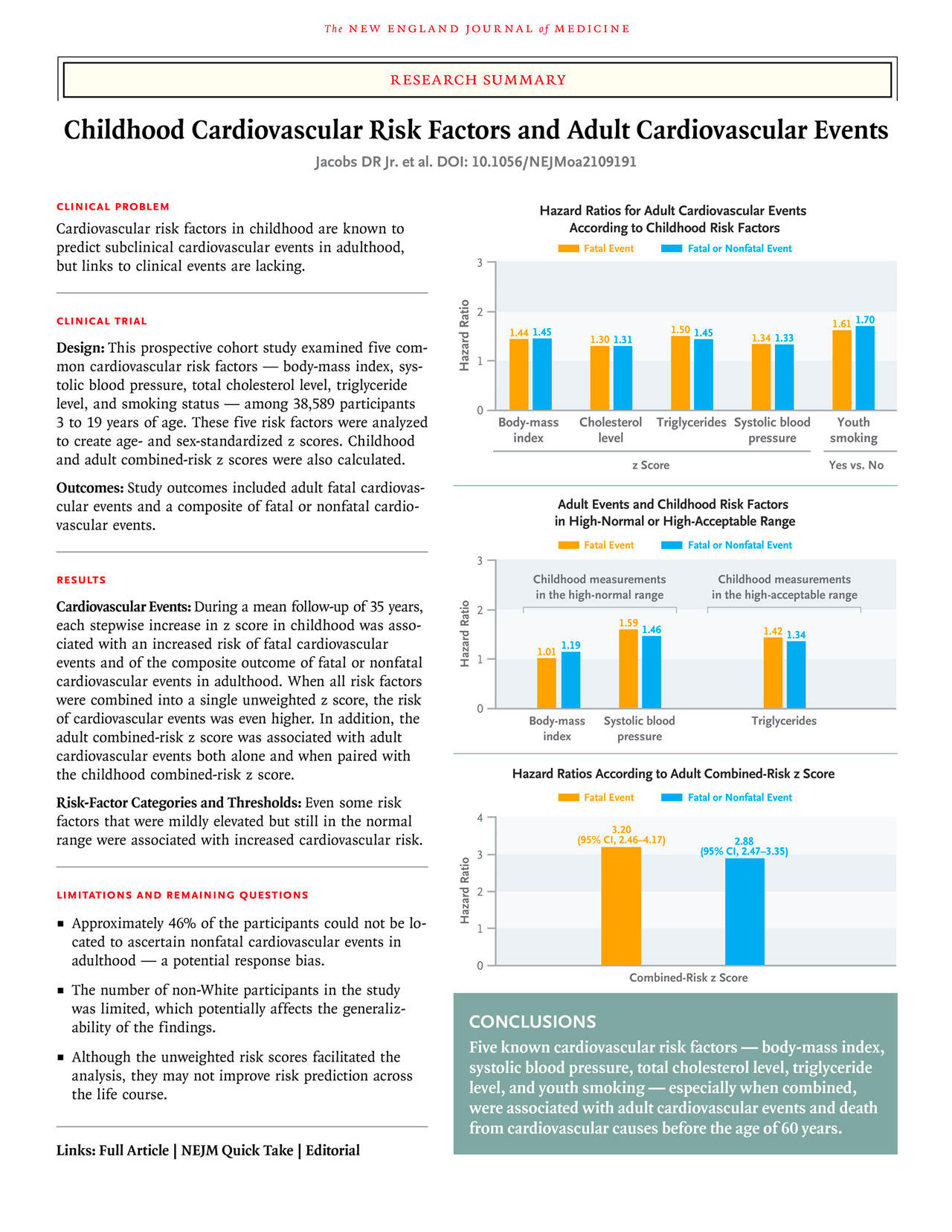
Childhood cardiovascular risk factors including BMI, systolic blood pressure, lipid levels, and smoking were correlated with cardiovascular events in adulthood after a mean follow-up of 35 years.
Childhood Cardiovascular Risk Factors and Adult Cardiovascular Events
BACKGROUND
Childhood cardiovascular risk factors predict subclinical adult cardiovascular disease, but links to clinical events are unclear.
METHODS
In a prospective cohort study involving participants in the International Childhood Cardiovascular Cohort (i3C) Consortium evaluating whether childhood risk factors (at the ages of 3 to 19 years) were associated with cardiovascular events in adulthood after a mean follow-up of 35 years. Body-mass index, systolic blood pressure, total cholesterol level, triglyceride level, and youth smoking were analyzed with the use of i3C-derived age- and sex-specific z scores and with a combined-risk z score that was calculated as the unweighted mean of the five risk z scores.
An algebraically comparable adult combined-risk z score (before any cardiovascular event) was analyzed jointly with the childhood risk factors.
The five risk factors were analyzed to create age- and sex-standarized z scores as well as childhood and adulthood combined-risk z scores were calculated
The five risk factors were analyzed to create age- and sex-standarized z scores as well as childhood and adulthood combined-risk z scores were calculated. Study outcomes were fatal cardiovascular events and fatal or nonfatal cardiovascular events, and analyses were performed after multiple imputation with the use of proportional-hazards regression.
RESULTS
In the analysis of 319 fatal cardiovascular events that occurred among 38,589 participants (49.7% male and 15.0% Black; mean [±SD] age at childhood visits, 11.8±3.1 years), the hazard ratios for a fatal cardiovascular event in adulthood ranged from 1.30 (95% confidence interval [CI], 1.14 to 1.47) per unit increase in the z score for total cholesterol level to 1.61 (95% CI, 1.21 to 2.13) for youth smoking (yes vs. no). The hazard ratio for a fatal cardiovascular event with respect to the combined-risk z score was 2.71 (95% CI, 2.23 to 3.29) per unit increase. The hazard ratios and their 95% confidence intervals in the analyses of fatal cardiovascular events were similar to those in the analyses of 779 fatal or nonfatal cardiovascular events that occurred among 20,656 participants who could be evaluated for this outcome. In the analysis of 115 fatal cardiovascular events that occurred in a subgroup of 13,401 participants (31.0±5.6 years of age at the adult measurement) who had data on adult risk factors, the adjusted hazard ratio with respect to the childhood combined-risk z score was 3.54 (95% CI, 2.57 to 4.87) per unit increase, and the mutually adjusted hazard ratio with respect to the change in the combined-risk z score from childhood to adulthood was 2.88 (95% CI, 2.06 to 4.05) per unit increase. The results were similar in the analysis of 524 fatal or nonfatal cardiovascular events.
CONCLUSIONS
In this prospective cohort study, childhood risk factors and the change in the combined-risk z score between childhood and adulthood were associated with cardiovascular events in midlife. (Funded by the National Institutes of Health.)
Predictors of Carotid Atherosclerosis in Young Adults: Insights From the Bogalusa Heart Study
Atherosclerotic cardiovascular disease (ASCVD) develops early in life, but becomes clinically manifest later on in adulthood. The Bogalusa Heart Study, which was initiated in 1972 by the pediatric cardiologist, Dr Gerald Berenson, and is still ongoing, has shown that ASCVD begins in childhood. In this issue of the Journal of the American Heart Association (JAHA), Razavi et al1 reported on the predictors of absence of carotid plaque among 508 young adult participants of the Bogalusa Heart Study, who underwent ultrasound imaging at baseline and a decade later. As expected, young age and a total cholesterol/high‐density lipoprotein cholesterol ratio <3.5 were associated with absence of plaque. Besides a favorable traditional risk factor profile and high glomerular filtration rate, they observed that low serum phosphate and calcium‐phosphate product and dietary sodium <2300 mg/d were associated with nondevelopment of plaque. This is a refreshing and important message, because it suggests that lifestyle changes early in life may protect against ASCVD many years later. However, because of the small sample size and the large number of variables collected, the findings would need to be confirmed in another cohort.
Dietary sodium intake is linked to the risk of developing hypertension2 and so the present study adds to the evidence supporting the current advice to cut sodium intake to <2300 mg/d. Nevertheless, a dietary sodium <2300 mg/d is substantially lower than the average sodium intake in the United States and other developed countries. Such a low intake is hard to sustain even in research studies. As a low sodium intake may activate the renin‐angiotensin system, Dr Michael Alderman and others have questioned whether this may be more harmful than beneficial.3 Moreover, a low sodium intake can be a marker of healthy diet or healthy lifestyle, because achieving a low sodium intake in Bogalusa would probably require fewer fast food meals and more fresh food ingredients.
Chronic kidney disease is well known to be associated with ASCVD, which is the leading cause of death in this patient group. Glomerular filtration rate and albuminuria are predictors of cardiovascular outcomes.4 Although the addition of glomerular filtration rate improves the prediction of cardiovascular events beyond traditional risk factors, it has not been included in popular cardiovascular risk scores, such as the Pooled Cohort Equation or the Systematic Coronary Risk Evaluation. Therefore, the study by Razavi et al confirms glomerular filtration rate as a predictor of carotid atherosclerosis independent of traditional risk factors. In young adults, a faster decline in the glomerular filtration rate may reflect the renal damage caused by chronically elevated blood pressure and glucose, especially when the young person is untreated.
In chronic kidney disease, serum calcium, phosphate, and the calcium‐phosphate product are elevated and are thought to contribute to arterial calcifications and cardiovascular events.5 Thus, phosphate binders are used clinically in patients with advanced chronic kidney disease, although it is still unclear whether non–calcium‐based phosphate binders are safer than calcium‐based phosphate binders in terms of cardiovascular outcome. Nevertheless, serum phosphate is also associated with vascular dysfunction and ASCVD, even in people without chronic kidney disease.6 Calcium‐phosphate homeostasis is tightly regulated by the levels of calcium, phosphate, parathyroid hormone, vitamin D, as well as newcomers, such as klotho and fibroblast growth factor 23, via the interplay between parathyroid gland, bone, kidney, and gut. The relationship between vitamin D and ASCVD has aroused much interest in the past decade. Circulating vitamin D levels were associated with a reduced risk of cardiovascular events in cohort studies7, 8; but clinical trials of vitamin D supplementation showed beneficial effects on cardiovascular risk factors only,9 but not on the incidence of CVD,10, 11 even with a high dose of vitamin D.12 Crucially, the VITAL (Vitamin D and Omega‐3 Trial) involving 25 871 participants followed up for 5 years found no benefit in vitamin D supplementation compared with placebo.13
Because other mineral markers are closely correlated with vitamin D levels, the association observed in those epidemiological studies could have been contributed by other minerals, such as calcium and phosphate. The role of calcium in ASCVD is intriguing. Two meta‐analyses by Ian Reid’s group showed that calcium supplementation increased the risk of myocardial infarction and cardiovascular diseases.14, 15 A Mendelian randomization study supported a possible casual role for serum calcium,16 although a subsequent meta‐analysis did not support a relationship between calcium supplementation and ASCVD.17 In the study by Razavi et al, serum phosphate and calcium‐phosphate product, but not serum calcium, were shown to be predictors of carotid atherosclerosis. Most of the previous studies on calcium‐phosphate and ASCVD risk were conducted in an older population and people with chronic kidney disease. The findings in the study by Razavi et al are of interest because these electrolyte measurements preceded clinical ASCVD. Interestingly, despite the difference in serum phosphate and calcium‐phosphate product, the baseline renal function was comparable between those with and without incident carotid atherosclerosis. This implies that young people with elevated phosphate and calcium‐phosphate product might be more prone to carotid atherosclerosis development. Further studies, using Mendelian randomization for instance, would be needed to establish causality.
The study by Razavi et al does not negate the importance of traditional risk factors. Although it showed that the 5 components of the metabolic syndrome could not explain nearly three quarters of the premature carotid atherosclerosis, age, smoking, blood pressure, low‐density lipoprotein, triglyceride, and waist circumference were all significantly associated with carotid atherosclerosis before multivariable adjustment. This brings home the point that ASCVD risk factors can be different in different age groups. Logically, the risk factors in the young are less likely to be diseases, such as hypertension and diabetes mellitus, but more likely to be related to genetics and lifestyle factors, including diet. Studies of ASCVD risk factors in children and young adults may reveal more novel risk factors and offer new approaches to stopping ASCVD before it develops.
Journal of the American Heart Association. 2021 – Footnotes

Go To Article